ASTHMA
Asthma
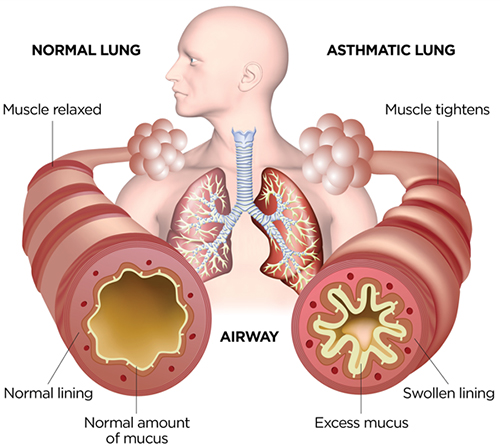
Asthma is a condition in which your airways narrow and swell and produce extra mucus. This can make breathing difficult and trigger coughing, wheezing and shortness of breath.
For some people, asthma is a minor nuisance. For others, it can be a major problem that interferes with daily activities and may lead to a life-threatening asthma attack.
- Causes of asthma
- Symptoms
- Asthma symptoms in children
- Asthma testing and diagnosis
- Asthma treatment
The fundamental causes of asthma are not completely understood. The strongest risk factors for developing asthma are a combination of genetic predisposition with environmental exposure to inhaled substances and particles that may provoke allergic reactions or irritate the airways, such as:
• indoor allergens (for example house dust mites in bedding, carpets and stuffed furniture, pollution and pet dander)
• outdoor allergens (such as pollens and moulds)
• tobacco smoke
• chemical irritants in the workplace
• air pollution
Other triggers can include cold air, extreme emotional arousal such as anger or fear, and physical exercise. Even certain medications can trigger asthma: aspirin and other non-steroid anti-inflammatory drugs, and beta-blockers (which are used to treat high blood pressure, heart conditions and migraine).
The most common signs of asthma are:
- coughing, especially at night, during exercise or when laughing
- Difficulty breathing
- Chest tightness
- Shortness of breath
- Wheezing (a whistling or squeaky sound in your chest when breathing, especially when exhaling)
Most children with asthma have symptoms before they turn 5. In very young children, it may be hard for parents, and even doctors, to recognize that the symptoms are due to asthma. The bronchial tubes in infants, toddlers and preschoolers are already small and narrow, and head colds, chest colds and other illnesses can inflame these airways, making them even smaller and more irritated.
The symptoms of pediatric asthma can range from a nagging cough that lingers for days or weeks to sudden and scary breathing emergencies.
Common symptoms to watch for include:
- coughing, especially at night
- A wheezing or whistling sound when breathing, especially when exhaling
- Trouble breathing or fast breathing that causes the skin around the ribs or neck to pull in tightly
- Frequent colds that settle in the chest
Your child might have only one of these symptoms or several of them. You may think it’s just a cold or bronchitis. If the symptoms recur, that’s a clue that your child might have asthma. In addition, symptoms may worsen when your child is around asthma triggers, such as irritants in the air (smoke or strong odors, for example) or allergens like pollen, pet dander and dust mites.
If you suspect you may have asthma, don’t let it keep you from your goals. And don’t feel like you have to face it alone. Teaming up with a pulmonologist is the secret to successfully managing your condition. A pulmonologist can evaluate your symptoms, make or confirm an asthma diagnosis and help you create a plan to manage your condition so you can live life to the fullest.
- Tests to measure lung function:
Spirometry: a small instrument that measures the amount of air you can breathe in and out. It’s a simple, safe test that helps measure how well your lungs are working.
You’ll be asked to breathe in until your lungs are full. You’ll then blow the air out into a hollow tube as hard and as fast as possible. The tube is attached to a device that measures how much air you’re able to hold in your lungs and detects whether anything is obstructing your airways.
Once you’ve taken the test once or twice, your pulmonologist may have you use an inhaler. You will then blow into the spirometer again to determine whether the inhaler medication improved your lung function.
Nitric oxide test: This test measures the amount of the gas, nitric oxide that you have in your breath. When your airways are inflamed — a sign of asthma — you may have higher than normal nitric oxide levels.
Allergy testing: This can be performed by a skin test. Allergy tests can identify allergy to pets, dust, mold and pollen. If important allergy triggers are identified, this can lead to a recommendation for allergen immunotherapy
Blood Test: is used to see if an individual’s blood contains antibodies for a specific substance, such as peanuts or pollen. These antibodies are called immunoglobulin E, or IgE antibodies
Imaging tests: A chest X-ray and high-resolution computerized tomography (CT) scan of your lungs and nose cavities (sinuses) can identify any structural abnormalities or diseases (such as infection) that can cause or aggravate breathing problems.
- Asthma diagnosis:
Your pulmonologist will look at your symptoms and family history, as well as the results of your physical exam and asthma testing, to determine if you have asthma. There are many different types of asthma, and each type can range from mild to moderate to severe.
If you receive an asthma diagnosis, don’t worry: Your pulmonologist can work with you to build a plan to control your symptoms and live the life you want.
Asthma is not a disability. With the right treatment, there’s no reason you can’t live life exactly as you would without this condition – sports, hiking, playing with your kids. You can have it all, as long as you get diagnosed and keep up with your treatment.
If you are like most people who have asthma, treatment can manage your symptoms, allow you to resume normal activities, and prevent asthma attacks. Treatment usually depends on your age, asthma severity, and your response to a given treatment option. Your doctor may adjust your treatment until asthma symptoms are controlled.
The treatment plan developed by your pulmonologist will address all your symptoms and will likely include at least one of the following:
- Identifying and then avoiding the specific triggers (such as tobacco smoke or pet dander) that bring on your symptoms.
- Medication, either over the counter or prescription including anti-histamines, inhalers, leukotriene inhibitors and biological therapy for severe asthma.
- Allergen immunotherapy (a highly effective preventive treatment that can help the immune system become less sensitive to triggers such as pollen, pet fur and house dust)












 أنقر هنا
أنقر هنا أنقر هنا
أنقر هنا